Prof. Dr. habil Levente Kovács, Dr. habil Tamás Ferenci
Main lines of research
- Evidence-based medicine
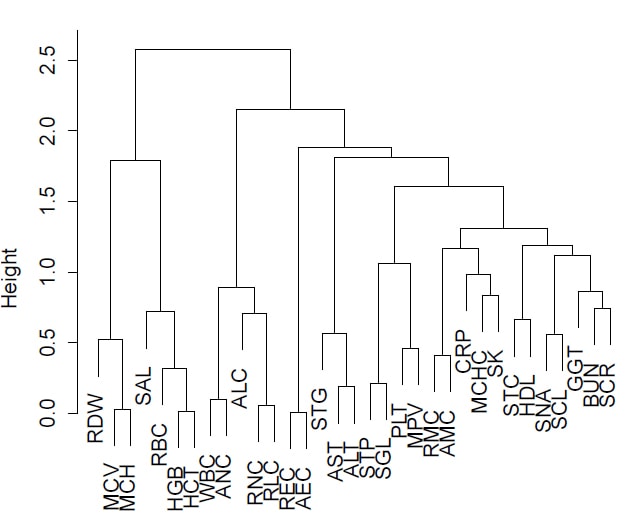
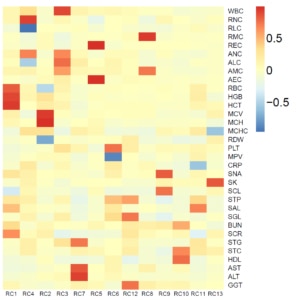
- Biostatistical evaluation of laboratory parameters in type I diabetes
- Epidemiological characteristics of major lower limb vascular diseases
Detailed description of the research
Biostatistics is an applied statistical field concerned with the quantitative study of biomedical questions involving empirical data. Does a new antihypertensive drug candidate actually lower blood pressure? Does living near high-voltage power lines really cause cancer? Is there a correlation between energy intake and height growth in children? These are just examples of questions that could be answered by using empirical data: collecting blood pressure data from people who do and do not take drugs, the distance of people’s homes from high-voltage power lines, and their cancer incidence and children’s height data. Using this data (if, of course, it were collected properly), we can hope to investigate problems and answer medically relevant questions.
Furthermore, it can be seen that all the examples lead to numerical data (blood pressure, cancer risk, height increase), so we can provide quantitative answers to the questions: what change in blood pressure does the drug cause, if any ; what percentage change in cancer risk is caused by living near a high voltage power line, if any; how does energy intake affect height increase, if it has any effect at all. To answer these questions, of course, we need to carry out appropriate studies (using the available data) and create the necessary models. This is what biostatistics deals with.
Modern medical research can hardly be imagined without the active involvement – or at least the support – of biostatistics. This is not surprising if we consider some of the trends in the development of medicine. Firstly, the empirical orientation has become increasingly pronounced over the past centuries and has been downright dominant during the 20th century. While anecdotal recollections of empirically driven medical research date back to biblical times, in the context of medicine before the 18th century there was no systematic, empirical thinking. (In 1747, James Lind conducted his sometimes questioned but nevertheless celebrated clinical experiment [1], in which he proved that scurvy could be treated with citrus fruits.)
This is not unconnected with the fact that it was at this time that a lasting body of knowledge was beginning to accumulate, both about the functioning of the healthy body and about its diseases. As for the former, it is related to the development of anatomy, especially because of the results of autopsies. (The only part that may be surprising is how long it took to correctly describe the most basic physiological functions in relation to the history of mankind; for example, the first essentially correct description of the human circulation was not given until 1628 [2]. (William Harvey.) As for the latter, at the same time, more modern, science-based theories began to replace earlier ideas about the causes of disease (bad air, gods, imbalance of humour, etc.) that are by today’s standards rather ridiculous.
From this point on, the empirical orientation only grew stronger and stronger, and it is perhaps not an exaggeration to say that this empirical orientation ended in the second half of the 20th century with the banning of evidence-based medicine [3] (whose key idea is to base clinical decision-making on the collection and critical evaluation of the best available scientific evidence – mostly the result of empirical studies.)
It should be noted that not only has the importance of empirical results (in general) increased, but also, specifically, the importance of quantitative results within them. This has been reinforced by the fact that the last decades of the 20th century have brought previously unimaginable computational capacity, applicable to both data processing and storage.
Another factor to consider is the progress of medicine towards a model-based approach. Traditionally, medical diagnosis has been distinguished from engineering diagnosis in that the latter has a precise model of how the failed object should work, unlike medicine, which has no arbitrarily detailed description of the “good” state. This is becoming less and less the case: advances in physiology have led to the development of clinically applicable models of such precision in many areas of medicine.
These were the precursors to the ‘medical side’ of biostatistics. The other side of the coin is the “mathematical side”.
The development of probability theory began in the 18th century (mainly thanks to the work of Jacob Bernoulli and Abraham de Moivre, and later Pierre-Simon de Laplace). By contrast, mathematical statistics, and in particular inferential statistics in their current form, only appeared at the end of the 19th and beginning of the 20th century [4, 5].
It is interesting to note that there was a significant motivation for this from applied science (although mostly due to agrometry – however, medicine also quickly joined the adopters). The pioneers were Ronald Aylmer Fisher, Jerzy Neyman and the two Pearsons, Karl and Egon.
The two developments (in medicine and in mathematical statistics) were “linked” in the 20th century. The results of mathematical statistics provided the methodological basis, while the development of medicine created the need for the application of the methods and procedures that we now collectively know as biostatistics.
Our research group conducts biostatistical studies on, among other things, laboratory parameters of obesity [6] and factors influencing blood glucose levels [7].
[1] Milne, Iain (2012). “Ki volt James Lind, és mit ért el pontosan”. In: Journal of the Royal Society of Medicine 105.12, 503–508. DOI: 10.1258 / jrsm.2012.12k090. eprint: http://jrs.sagepub.com/content/105 /12/503.full.pdf+html . URL: http://jrs.sagepub.com/content/105/12/503 . rövid .
[2] Sloan, AW (1978). – William Harvey, orvos és tudós. In: Dél-afrikai orvosi folyóirat 54.6, p. 247.
[3] Sackett, David L, William M C Rosenberg, J A Muir Gray, R Brian Haynes és W Scott Richardson (1996). „Bizonyítékokon alapuló orvoslás: mi ez és mi nem”. In: British Medical Journal 312.7023, 71–72. DOI: 10.1136 / bmj.312.7023.71.
[4] Hald, Anders (2003). A valószínűség és a statisztika története és alkalmazásuk 1750 előtt. John Wiley & Sons, ISBN: 9780471471295.
[5] Hald, Anders (1998). A matematikai statisztika története 1750 és 1930 között . John Wiley & Sons. ISBN: 9780471179122.
[6] Ferenci, Tamás (2013). A biostatisztika két alkalmazása a kórélettani folyamatok elemzésében . Doktori (PhD) értekezés tétele, Obudai Egyetem.
[7] Ferenci, Tamás, Körner, Anna and Kovács, Levente (2013). „Korrelációs vizsgálatok a HbA1c és a vércukorszint mutatói között az 1-es típusú cukorbeteg magyar gyermekeknél”. In: Szakál Anikó (szerk.) SACI 2013 – 8. Nemzetközi Szimpózium az alkalmazott számítástechnikai intelligenciáról és informatikáról . 443-447. ISBN: 978467364003.